Key Takeaways
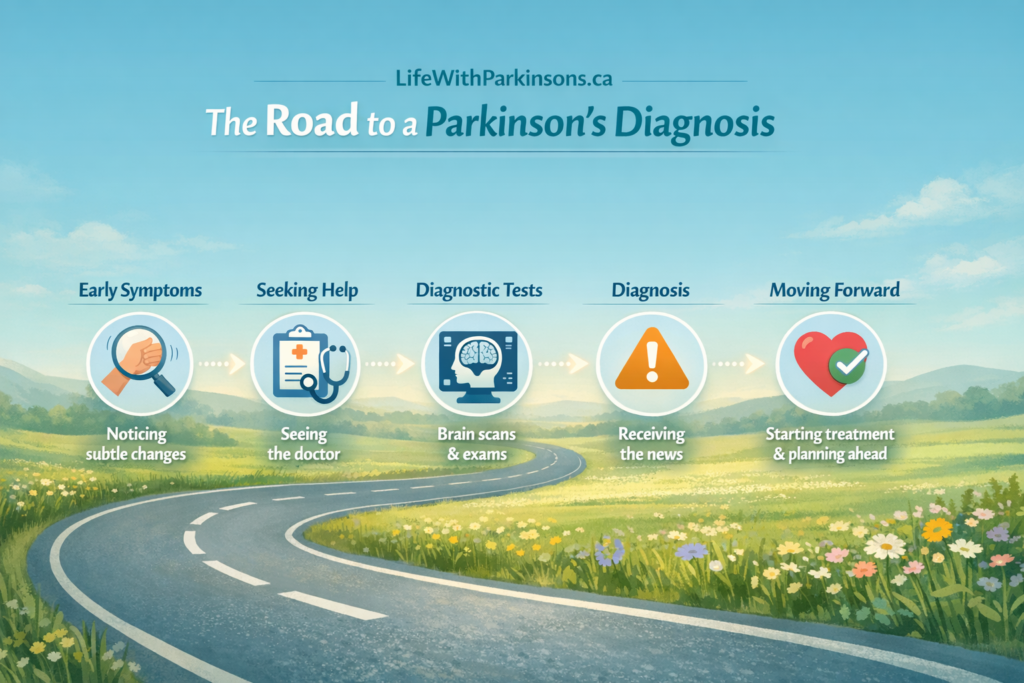
- Early symptoms can be subtle and easy to dismiss, but noticing small changes and trusting your instincts can make a real difference.
- A Parkinson’s diagnosis often comes with shock and uncertainty—this reaction is normal, and you are not alone in feeling it.
- Understanding what to expect during doctor visits and diagnostic tests can reduce fear and help you advocate for yourself or a loved one.
- Combining personal experience with reliable information can offer clarity, reassurance, and practical guidance during an overwhelming time.
- Sharing stories helps others recognize symptoms sooner, prepare emotionally, and navigate the journey with more confidence and support.
1. Introduction: The Diagnosis That Changed Everything
Hi, I’m David Gebhart. I’m 44 years old and live in British Columbia. Back in May 2017, I was finally diagnosed with Parkinson’s disease. It was the culmination of a five-year journey from first symptoms to an answer. My type of Parkinson’s is more movement-related than tremor-based – I do tremble when I’m nervous, but stiffness and rigidity are what really hit my life hard. When the neurologist gently said “you have parkinsonism” and then gave me a test medication (Sinemet), everything went quiet around me. In that instant I knew life had changed forever.
Looking back, my goal now is to turn that shock into guidance. I want to share the full story of how I got here – from subtle early signs through the doctor visits and tests – so that others can recognize symptoms sooner and know what to expect. By putting my personal journey together with facts and tips, I hope this guide helps you or someone you love navigate the road ahead.
2. The “Invisible” Years: Non-Motor Symptoms I Missed

The Anxiety Factor
In the years before my diagnosis, I noticed things that didn’t quite add up – like crippling anxiety at work and in public speaking. For example, early on I’d feel unusually nervous about presentations, and even my fine hand movements would freeze up in stressful moments. I now know that anxiety and mood changes are common “invisible” symptoms of Parkinson’s. At the time, I just thought the pressure of a management job and public speaking was getting to me. In reality, those anxiety attacks and sweatiness were early warning signs of PD. (Research confirms that mood disturbances and anxiety can emerge long before the classic movement issues.)
Sleep Disturbances
Another subtle clue was my sleep. I’d wake up exhausted most mornings or fall into deep naps during the day. Occasionally, I’d have vivid, troubling dreams – nightmares so intense they’d wake me gasping. I brushed these off for years. Only later did I learn that Parkinson’s often causes sleep problems and even REM sleep behavior disorder (acting out dreams). It turns out my nightly leg jerks and fatigue weren’t just fatigue – they were part of the disease lurking under the surface.
Loss of Smell
One classic early symptom I completely ignored was smell loss. Around 2015 I realized I couldn’t smell things I used to – I couldn’t detect propane leaks, trash odors, or even strong soaps. My coworkers would joke about funny smells I didn’t notice. I just thought I had allergies or a cold. Little did I know, decreased ability to smell is a well-known non-motor sign of Parkinson’s. Parkinson’s affects the olfactory nerves early on, and over time I lost most of my sense of smell without even realizing it.
Looking back, these “invisible” symptoms – anxiety, terrible dreams, fatigue, and a fading sense of smell – were my first clues. But because none of them looked like shaking or a limp, I missed the pattern. If you’re experiencing similar issues, it’s worth noting that many people with early Parkinson’s report exactly these signs.
3. The Visible Shift: When My Body Started Changing (Motor Symptoms)

The Left Side Lag
By 2013 I began to notice physical changes. My left hand – the one I write and screw bolts with – started moving strangely. I remember telling myself, “Come on, left hand, you can do this,” while I tried to grip small screws or open jars. My co-workers were patient, but I felt clumsy. Simple tasks like screwing a bolt became frustratingly hard. Looking back, this loss of fine motor control in my left hand was a clear sign of Parkinson’s bradykinesia – slowness of movement on one side. Because it was gradual, I hardly noticed at first, but it was the beginning of a slow drag on my left side.
The “Social Mirror” (Lack of Arm Swing)

Sometimes others noticed changes I didn’t see myself. In March 2017, I went to a family funeral thinking I could hide my stiffness. I felt pretty normal, just a bit sore. But then my uncle quietly asked my parents, “Is there something wrong with David? He doesn’t look well.” I didn’t realize what he saw, but later I understood: when I walked, my left arm no longer swung naturally – it hung stiff at my side. In healthy walking, people’s arms swing opposite their legs. Mine didn’t, and a sharp eye in the family “social mirror” picked it up before I did. That was an unsettling wake-up call – even when I tried to mask it, my body was moving differently, and others could see it.
The Limp
Over the next year, I even developed a subtle limp in my left leg. At first I blamed my old right ankle injury and surgery. But it made no sense: why would one old foot injury cause my opposite leg to drag? By 2015, I had a noticeable shuffle and limp on the left side, especially when I was tired. I was in my late 30s and knew it wasn’t normal aging or job strain (I had a physically demanding job as an overhead door technician). All these motor changes – the weak grip, the stiff left arm swing, the dragging left leg – kept happening on one side. They were the visible shift I couldn’t ignore any longer.
4. The Turning Point: “Are You Stiff?”
The GP Visits
Throughout this time I saw my family doctor often. Funny thing – it was originally for something unrelated (plantar warts on my left foot!). But every appointment, my doctor took note. He’d glance as I walked to the exam room or had me bend and lift my arms. He’d pause when I sat down and smile awkwardly: “David, are you feeling stiff lately?” Over weeks, I felt increasingly frustrated that my body was betraying me, but the warts visit became the moment those clues added up.
The Referral
Finally, on May 28, 2017, my doctor made a bold move: he urgently referred me to a neurologist for evaluation. It was a Sunday appointment – very unusual, but he insisted I be seen immediately. That Sunday visit was a turning point. At last, a specialist would look at all these signs – the stiffness, the left-sided symptoms, and my own list of odd symptoms – to figure out what was happening.
5. Inside the Neurologist’s Office: How Parkinson’s is Diagnosed
When I walked into the neurologist’s office, I was nervous but relieved to finally have answers in sight. He explained the process: a three-part evaluation.

The Questionnaire
First came a detailed questionnaire. The neurologist asked about toxins, pesticides, head injuries, and even alcohol or drug use. Then he asked something unexpected: dreams. “Do you have violent or vivid dreams?” he asked. I was surprised, but I admitted I had been having night terrors lately. That discussion immediately connected dots. He next asked about my sense of smell – and in that moment I realized, of course I had lost my smell too (something I hadn’t fully noticed until he pointed it out). He also checked family history (I mentioned a great-uncle who might have had it) and past injuries (a bad ladder fall requiring foot surgery). All these questions were standard: Parkinson’s is diagnosed clinically, by asking about symptoms and history.
The Physical Exam
Next was the physical exam. He had me walk up and down the hallway so he could watch my gait. As I walked, my left arm remained unnaturally still at my side – no swinging at all. He had me do small movements: snap my fingers, flip my hands over, and touch my nose. He noted that I was slower and less precise on the left. He also did reflex tests on my knees and elbows. At one point he gave me a cold object to feel and asked me to compare both hands; interestingly, my left hand hardly felt the cold.
Then came classic Parkinson’s checks: he had me tap my index finger to my thumb repeatedly and watch closely (a common bradykinesia test). He tested my wrist and elbow passively for rigidity (checking muscle tone). To check rigidity, he felt my wrist and elbow as I relaxed, and I could feel the pull as he moved them – my left side felt stiff, like a “lead-pipe” resistance. He did the same on my leg and ankle, turning and flexing them to compare both sides. Throughout, I kept thinking how thorough he was: “hmm…” he’d murmur, taking it all in.
The “Sinemet Test”
Finally, the neurologist was very careful with the diagnosis. He told us he first had to rule out other conditions. He ordered multiple blood tests (filling six vials in the lab form!) and even scheduled an MRI, just to be sure nothing else was causing these symptoms. In fact, he referred me to a second neurologist for another opinion – which confirmed his suspicions.
Then he said something that finally felt like an answer: “We’ll do a medication test.” He wrote a prescription for Sinemet (levodopa/carbidopa) – a gold-standard PD treatment. He explained that if the medication improved my symptoms, it would strongly suggest Parkinson’s. I started the pills the next morning, and within hours I noticed my left arm loosening, my steps feeling smoother. It was a confirmation: I did have Parkinson’s. All those missed signs now made sense.
6. Processing the News: The First 24 Hours
When the word finally came – that I had Parkinson’s disease – it hit me like a wave. My mind went blank and my heart sank. My wife and I sat in silence for a moment. I felt strange relief (the uncertainty was over) and deep fear (what would this mean?). In the first hours, we cried, held each other, and asked endless questions: What does our future look like? How do we tell our kids?

That night I couldn’t sleep. I read articles and videos online, feeling nervous but also grateful. My family was supportive; my wife promised we’d face it together. Later, even people who knew me well expressed shock. But some also offered hope: as one doctor said, the first few years after diagnosis can be a “honeymoon stage” where medication works well. We clung to that.
By dawn, we had a plan: I would start medication, keep a positive mindset, and look into exercise and support groups. It was the beginning of accepting this new reality. We were terrified and heartbroken, but also oddly hopeful that knowledge is power.
8. Resources & Next Steps
If you or a loved one are navigating a Parkinson’s diagnosis, you are not alone. Here are some trusted resources and first steps:
- Michael J. Fox Foundation for Parkinson’s Research: The MJFF website has excellent guides on symptoms, diagnosis, and living well with Parkinson’s (see the Symptoms page and Exercise guide). For example, they note that “Exercise is one of the most powerful treatments for Parkinson’s disease” and can even help slow progression and improve balance and strength.
- Parkinson’s Canada: For Canadians, Parkinson.ca offers education, support programs, and guides on everything from early symptoms to fitness and nutrition. (The US Parkinson’s Foundation has similar resources, including starter kits and community support.)
- Exercise for Parkinson’s: Staying active is crucial. Aerobic exercises (like walking, cycling or dance) and strength/balance exercises can improve mobility and mood. I write about exercise routines on my site, and MJFF has a handy Exercise resource summarizing the benefits.
- Nutrition: Good nutrition supports brain health and medication effectiveness. On my blog I’ve shared tips about diet and timing of meals (e.g. managing protein intake so your Sinemet works well). Parkinson’s organizations also offer diet guides (for example, strategies to make levodopa more effective with meals).
Exercise is often cited as one of the best tools in Parkinson’s management, helping with strength, balance, mood, and even slowing disease progression. Error! Filename not specified.
- Support groups and counseling: Emotional support is vital. Look for local Parkinson’s support groups (in-person or online) where you can share experiences. If possible, involve family and friends early – they can be your best advocates (my uncle prompted my diagnosis) and support system.
Take it one step at a time. Stay informed, keep moving, and reach out for help when you need it. There are research foundations, community organizations, and many online forums full of people who know exactly what you’re going through. You’ll also find resources on daily exercises and nutrition tips at sites like the Michael J. Fox Foundation and Parkinson’s Canada. Building a healthcare team (GP, neurologist, physical therapist, counselor) early can make a big difference in quality of life.
Medical Disclaimer: I am not a medical professional. This post is based on my personal experience and research. Parkinson’s symptoms and progression vary widely from person to person. If you or a loved one are noticing symptoms, please consult a qualified doctor. Early evaluation by a neurologist or movement disorder specialist is important. For reliable information, see organizations like the Parkinson’s Foundation or Michael J. Fox Foundation
A Note for Caregivers
If you’re reading this as a spouse, partner, family member, or close friend, your role in this journey matters more than you may realize. Many of the earliest signs of Parkinson’s — changes in mood, memory, sleep, or movement — are often noticed by caregivers before the person experiencing them fully recognizes what’s happening.
Your observations, patience, and support can help shorten the path to diagnosis and make the early stages far less frightening. Parkinson’s doesn’t just affect one person — it affects the entire family. Make sure you take care of yourself too, ask questions during medical appointments, and seek support when you need it. You are not “on the sidelines” of this journey — you are an essential part of it.